Pucker Up 4 PAH Interview

Pucker Up 4 PAH Interviews
Give us a blue-lipped kiss - and learn more about PAH (Pulmonary Arterial Hypertension)!
This November, use your lips to pucker up and talk about Pulmonary Arterial Hypertension (PAH), an uncommon but life-threatening disease.
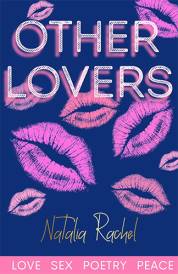
PuckerUp4PH is a global awareness-raising campaign born out of the UK and now is a global initiative. The 2010 aim is to help set a new Guinness World Record by obtaining 40,000 blue lip stick prints from people around the world™.
Blue lips is an inspirational motif for PuckerUP4PH as blue lips, or cyanosis as it's medically termed, can be a symptom of PAH.
PHA Australia, the organisation representing PAH patients in Australia, endorses this campaign and encourages all Australians to pucker up for PAH.
Joan Godber, President, PHA Australia believes "the PuckerUp4PH campaign will help to raise vital awareness of PAH around the world as well as provide much-needed understanding of the disease here in Australia."
It's estimated that there are currently 100,000 people worldwide with PAH.
PAH symptoms can include breathlessness and fatigue in addition to the blue lips. Breathlessness is a key symptom of PAH and is often what causes people to seek treatment.
Professor Anne Keogh, explains PAH:
"PAH is a devastating disease characterised by high blood pressure in the pulmonary arteries leading to heart failure, even death. It is marked by elevated blood pressure in the lung's arteries, putting pressure on the heart and reducing the amount of oxygen able to reach the tissues of the body. It leads to breathlessness which often leaves patients with the inability to exercise or do even the simplest tasks. Without treatment and the proper medication, the prognosis is not good.
"PAH can affect males and females, adults and children, of all ages and ethnic backgrounds. But it does seem to be most common in those aged between 20-40 years and there are nearly twice as many females as males with the condition.
"PAH is often misdiagnosed and often symptoms do not become apparent until the disease has advanced. In the early stages of PAH, symptoms and signs can be confused with other conditions affecting the heart and lungs like asthma. A number of tests can be used to assist in the diagnosis of PAH with the definitive test being a right heart catheterisation. Navigating a patient through a battery of tests can be a difficult journey."
Due to the non-specific nature of the symptoms, PAH is most frequently diagnosed when patients have reached an advanced state of the disease (WHO functional Class III and IV), suggesting that the true prevalence may be higher than documented in the literature.
However, Professor Keogh is extremely hopeful.
"Currently there are very effective treatments available to help PAH patients manage their quality of life. Of course everyone reacts differently, which is why there are a number of different medications and clinical trials are taking place all the time. We're feeling more positive about PAH treatment now."
In Australia the PuckerUp4PH campaign is supported by PHA Australia, Professor Anne Keogh and Pfizer Australia.
PuckerUp4PH is a global initiative developed in the United Kingdom but is now associated with 29 pulmonary hypertension patient groups across the world including Australia and New Zealand. Puckerup4PH is an annual awareness raising campaign for pulmonary arterial hypertension (PAH), a heart/lung disorder. It's estimated that there are currently 100,000 people worldwide with PAH. The Blue Lips logo was developed to help improve awareness of the condition globally both in the public consciousness and within the healthcare profession.
What is PAH?
Pulmonary arterial hypertension (PAH) is a rare, devastating and life threatening disease characterised by high blood pressure in the pulmonary arteries, leading to heart failure and premature death. These major blood vessels carry blood from the heart to the small blood vessels in the lungs, where oxygen exchange takes place. PAH is a chronic, progressively deteriorating disease that requires medical treatment. The increased pressure in the pulmonary arteries makes the heart work much harder as it tries to move blood through these arteries. This puts a strain on the right side of the heart.
What are the causes?
There are three different types of PAH:
PAH caused by other conditions, such as connective tissue diseases (e.g. scleroderma or lupus), congenital heart disease, liver disease, or HIV or certain drugs
PAH with no known cause (idiopathic PAH)
PAH that affects multiple family members (familial PAH).
Who is affected?
There are about 100,000 people with PAH worldwide.
PAH affects males and females - adults and children - of all ages and ethnic backgrounds. Although it can affect all age groups and both genders, PAH is common in those aged between 20-40 years and there are nearly twice as many females as males with the condition.
What are the symptoms?
Symptoms of PAH often do not become obvious until the pulmonary disease progresses. In most patients, the signs and symptoms of PAH are not easily recognised. The earliest symptoms of PAH are often confused with asthma. Therefore, people diagnosed with asthma, who have not responded to treatment after several years, should be tested for PAH.
Early symptoms may include:
Shortness of breath (also called dyspnoea)
Fatigue
Chest pain, especially when exercising
Heart palpitations
Swollen ankles (also called oedema)
Dizziness and/or feeling lightheaded
Fainting (also called syncope).
As the disease progresses, these symptoms may become more noticeable, and you may find it harder to do everyday activities.
How is it diagnosed?
PAH is often misdiagnosed and often occurs late in the disease stage as symptoms and signs are confused with other conditions affecting the heart and lungs. For example, shortness of breath is more often attributed to asthma and tends to be the first and more frequent diagnosis. As a result, patients with PAH may receive delayed PAH treatment.
A number of tests can be used to assist in the diagnosis of PAH and exclusion of other diseases.
An echocardiogram (ultrasound of the heart), chest X Ray, electrocardiogram, followed by breathing tests, walking tests (6 minute walk test), CT scan of the lungs, lung function tests can be useful tests for PAH.
However, the definitive test for PAH is a right heart catheterisation. Doctors have devised a classification system to help understand to what extent the PAH symptoms are affecting daily activities. The classification is based on the severity of symptoms and is referred to as a PAH "functional class." Knowing a patient's functional class- anywhere from class I to class IV, where class I is very early stage PAH and a functional class of IV is very severe PAH - helps the doctor determine which type of treatment should be given.
What is the outlook for PAH patients?
As patients are often diagnosed late or remain undiagnosed, the prognosis is poor. Prior to the availability of current PAH-specific therapy, idiopathic PAH patients had a median survival time from 2.8 years from the time of diagnosis.
The aim is to ensure diagnosis of PAH occurs earlier in the disease so that PAH therapy may lead to better patient outcomes.
How patients are currently treated?
There are very effective treatments available for PAH including oral tablets, inhaled and intravenous (IV) medications.
Common treatments include:
Anticoagulants, such as warfarin, which help to thin the blood and prevent blood clots from forming
Medicines that relax the blood vessels in your lungs, and/or help to prevent vascular remodelling in the lungs (e.g. phosphodiesterase- 5 inhibitors, prostanoids, endothelin receptor antagonists, and calcium channel blockers)
Oxygen therapy, to increase your blood oxygen supply
Diuretics, or "water pills", which reduce fluid build-up in the body
Digoxin, which helps the heart to beat more strongly and pump more blood.
Goals of treatment
There is not yet a cure for PAH. The goals of treatment are to:
Improve quality of life
Stabilise and improve symptoms
Slow down the progression of the disease.
For more information, please visit:
www.phaaustralia.com.au
www.phnsw.org.au
www.lungfoundation.com.au
www.puckerup4ph.com

This November, use your lips to pucker up and talk about Pulmonary Arterial Hypertension (PAH), an uncommon but life-threatening disease.
PuckerUp4PH is a global awareness-raising campaign born out of the UK and now is a global initiative. The 2010 aim is to help set a new Guinness World Record by obtaining 40,000 blue lip stick prints from people around the world™.
Blue lips is an inspirational motif for PuckerUP4PH as blue lips, or cyanosis as it's medically termed, can be a symptom of PAH.
PHA Australia, the organisation representing PAH patients in Australia, endorses this campaign and encourages all Australians to pucker up for PAH.
Joan Godber, President, PHA Australia believes "the PuckerUp4PH campaign will help to raise vital awareness of PAH around the world as well as provide much-needed understanding of the disease here in Australia."
It's estimated that there are currently 100,000 people worldwide with PAH.
PAH symptoms can include breathlessness and fatigue in addition to the blue lips. Breathlessness is a key symptom of PAH and is often what causes people to seek treatment.
Professor Anne Keogh, explains PAH:
"PAH is a devastating disease characterised by high blood pressure in the pulmonary arteries leading to heart failure, even death. It is marked by elevated blood pressure in the lung's arteries, putting pressure on the heart and reducing the amount of oxygen able to reach the tissues of the body. It leads to breathlessness which often leaves patients with the inability to exercise or do even the simplest tasks. Without treatment and the proper medication, the prognosis is not good.
"PAH can affect males and females, adults and children, of all ages and ethnic backgrounds. But it does seem to be most common in those aged between 20-40 years and there are nearly twice as many females as males with the condition.
"PAH is often misdiagnosed and often symptoms do not become apparent until the disease has advanced. In the early stages of PAH, symptoms and signs can be confused with other conditions affecting the heart and lungs like asthma. A number of tests can be used to assist in the diagnosis of PAH with the definitive test being a right heart catheterisation. Navigating a patient through a battery of tests can be a difficult journey."
Due to the non-specific nature of the symptoms, PAH is most frequently diagnosed when patients have reached an advanced state of the disease (WHO functional Class III and IV), suggesting that the true prevalence may be higher than documented in the literature.
However, Professor Keogh is extremely hopeful.
"Currently there are very effective treatments available to help PAH patients manage their quality of life. Of course everyone reacts differently, which is why there are a number of different medications and clinical trials are taking place all the time. We're feeling more positive about PAH treatment now."
In Australia the PuckerUp4PH campaign is supported by PHA Australia, Professor Anne Keogh and Pfizer Australia.
PuckerUp4PH is a global initiative developed in the United Kingdom but is now associated with 29 pulmonary hypertension patient groups across the world including Australia and New Zealand. Puckerup4PH is an annual awareness raising campaign for pulmonary arterial hypertension (PAH), a heart/lung disorder. It's estimated that there are currently 100,000 people worldwide with PAH. The Blue Lips logo was developed to help improve awareness of the condition globally both in the public consciousness and within the healthcare profession.
What is PAH?
Pulmonary arterial hypertension (PAH) is a rare, devastating and life threatening disease characterised by high blood pressure in the pulmonary arteries, leading to heart failure and premature death. These major blood vessels carry blood from the heart to the small blood vessels in the lungs, where oxygen exchange takes place. PAH is a chronic, progressively deteriorating disease that requires medical treatment. The increased pressure in the pulmonary arteries makes the heart work much harder as it tries to move blood through these arteries. This puts a strain on the right side of the heart.
What are the causes?
There are three different types of PAH:
PAH caused by other conditions, such as connective tissue diseases (e.g. scleroderma or lupus), congenital heart disease, liver disease, or HIV or certain drugs
PAH with no known cause (idiopathic PAH)
PAH that affects multiple family members (familial PAH).
Who is affected?
There are about 100,000 people with PAH worldwide.
PAH affects males and females - adults and children - of all ages and ethnic backgrounds. Although it can affect all age groups and both genders, PAH is common in those aged between 20-40 years and there are nearly twice as many females as males with the condition.
What are the symptoms?
Symptoms of PAH often do not become obvious until the pulmonary disease progresses. In most patients, the signs and symptoms of PAH are not easily recognised. The earliest symptoms of PAH are often confused with asthma. Therefore, people diagnosed with asthma, who have not responded to treatment after several years, should be tested for PAH.
Early symptoms may include:
Shortness of breath (also called dyspnoea)
Fatigue
Chest pain, especially when exercising
Heart palpitations
Swollen ankles (also called oedema)
Dizziness and/or feeling lightheaded
Fainting (also called syncope).
As the disease progresses, these symptoms may become more noticeable, and you may find it harder to do everyday activities.
How is it diagnosed?
PAH is often misdiagnosed and often occurs late in the disease stage as symptoms and signs are confused with other conditions affecting the heart and lungs. For example, shortness of breath is more often attributed to asthma and tends to be the first and more frequent diagnosis. As a result, patients with PAH may receive delayed PAH treatment.
A number of tests can be used to assist in the diagnosis of PAH and exclusion of other diseases.
An echocardiogram (ultrasound of the heart), chest X Ray, electrocardiogram, followed by breathing tests, walking tests (6 minute walk test), CT scan of the lungs, lung function tests can be useful tests for PAH.
However, the definitive test for PAH is a right heart catheterisation. Doctors have devised a classification system to help understand to what extent the PAH symptoms are affecting daily activities. The classification is based on the severity of symptoms and is referred to as a PAH "functional class." Knowing a patient's functional class- anywhere from class I to class IV, where class I is very early stage PAH and a functional class of IV is very severe PAH - helps the doctor determine which type of treatment should be given.
What is the outlook for PAH patients?
As patients are often diagnosed late or remain undiagnosed, the prognosis is poor. Prior to the availability of current PAH-specific therapy, idiopathic PAH patients had a median survival time from 2.8 years from the time of diagnosis.
The aim is to ensure diagnosis of PAH occurs earlier in the disease so that PAH therapy may lead to better patient outcomes.
How patients are currently treated?
There are very effective treatments available for PAH including oral tablets, inhaled and intravenous (IV) medications.
Common treatments include:
Anticoagulants, such as warfarin, which help to thin the blood and prevent blood clots from forming
Medicines that relax the blood vessels in your lungs, and/or help to prevent vascular remodelling in the lungs (e.g. phosphodiesterase- 5 inhibitors, prostanoids, endothelin receptor antagonists, and calcium channel blockers)
Oxygen therapy, to increase your blood oxygen supply
Diuretics, or "water pills", which reduce fluid build-up in the body
Digoxin, which helps the heart to beat more strongly and pump more blood.
Goals of treatment
There is not yet a cure for PAH. The goals of treatment are to:
Improve quality of life
Stabilise and improve symptoms
Slow down the progression of the disease.
For more information, please visit:
www.phaaustralia.com.au
www.phnsw.org.au
www.lungfoundation.com.au
www.puckerup4ph.com

Interview with Professor Anne Keogh
Professor Anne Keogh is the Senior Cardiologist in the Transplant Unit and Head of Clinical Research at St Vincent's Hospital, Sydney.
Question: Why is PuckerUp4PH important for you?
Professor Anne Keogh: PuckerUp4PH is a UK initiative that aims to improve awareness for PAH and this is the first time Australia has had an involvement in this campaign. We have piggy backed on to improve awareness for PAH. There is an attempt for 40,000 big blue lips to gain attention and to place in the Guinness Book of World Records.
The idea is to improve people's awareness of breathlessness and to not always attribute it to being overweight, getting older or other issues and to show that it is important to get a medical opinion about the breathlessness.
People and doctors need to understand the symptoms and realise that this is serious and has a diagnoses rate worse than cancer.
In the last decade there have been advantages in treatments in terms of drips and medicine but the diagnoses is still worse than cancer as the delay from when people become breathless to the diagnoses and being mediated is about three years and that is unacceptable. Awareness for PAH is needed.
Many doctors don't know a lot about PAH and that is because when they were at school it was seen as an untreatable. Many of the advantages in terms of treatment have been discovered over the last decade.
Question: How can Australia get involved in PuckerUp4PH?
Professor Anne Keogh: By going to the website which is quite good fun, there are fun cartoons and excellent links to patients and their stories with simple explanations and stories of people who were ill and are now back to a close-to-normal life.
You can join in with the blue lips and send them off to other people, to raise awareness. Of course, that's the catchy side of the campaign. PuckerUp4PH is about the disease and the patients and ensuring they're correctly diagnosed.
Question: What is PAH?
Professor Anne Keogh: We now understand high blood pressure and PAH is high blood pressure of the lung circuit. High blood pressure of the lung circuit is dangerous as it damages the walls of the arteries and people eventually become unable to breathe and go into heart failure, they then die of heart failure.
Question: Why are people who have PAH often not aware of it?
Professor Anne Keogh: Mostly because it has only been in the last decade that there have been therapies' and attempts to find patients with PAH.
About 3,500-4,000 people have PAH, in Australia and not even half of them are being treated; we know this from a Western Australia PhD study by Mr. Strange. He looked at what the magnitude in a certain population was and half the people in that population that had PAH were not being treated.
PAH is quite a hard disease to diagnose, unless the doctors are looking for it.
Question: How does PAH affect ones daily life?
Professor Anne Keogh: Breathlessness and tiredness- which is why PAH can be cheeky to diagnoses because everyone feels tired at times.
Question: What can PAH patients do to manage their lives?
Professor Anne Keogh: Mother's might have trouble looking after their kids and older people make have trouble with daily activities such as talking on the phone, showering and walking from room to room. Getting onto therapies and exercise programs can help with the symptoms of PAH.
Question: How can you manage PAH?
Professor Anne Keogh: Mainly with medication to bring the blood pressure of the lungs down. It is critical that a patient starts as soon as possible because if it is left unattended it has a bad outlook as most are dead within 2 or 3 years. It is important to hop in and treat PAH as soon as breathlessness arises.
Lupus and Scleredema sufferers and their specialists need to be aware of PAH and be checked out for PAH each year, by specialists looking and organising an echo soundwave test on the heart. 1 in 5 Scleredema patients have PAH. Lupus and Scleredema patients need to be aware of PAH and ask their specialist (cardiologist) to test for it. The echo soundwave test on the heart will point to or away from the diagnoses.
Interview by Brooke Hunter
Question: Why is PuckerUp4PH important for you?
Professor Anne Keogh: PuckerUp4PH is a UK initiative that aims to improve awareness for PAH and this is the first time Australia has had an involvement in this campaign. We have piggy backed on to improve awareness for PAH. There is an attempt for 40,000 big blue lips to gain attention and to place in the Guinness Book of World Records.
The idea is to improve people's awareness of breathlessness and to not always attribute it to being overweight, getting older or other issues and to show that it is important to get a medical opinion about the breathlessness.
People and doctors need to understand the symptoms and realise that this is serious and has a diagnoses rate worse than cancer.
In the last decade there have been advantages in treatments in terms of drips and medicine but the diagnoses is still worse than cancer as the delay from when people become breathless to the diagnoses and being mediated is about three years and that is unacceptable. Awareness for PAH is needed.
Many doctors don't know a lot about PAH and that is because when they were at school it was seen as an untreatable. Many of the advantages in terms of treatment have been discovered over the last decade.
Question: How can Australia get involved in PuckerUp4PH?
Professor Anne Keogh: By going to the website which is quite good fun, there are fun cartoons and excellent links to patients and their stories with simple explanations and stories of people who were ill and are now back to a close-to-normal life.
You can join in with the blue lips and send them off to other people, to raise awareness. Of course, that's the catchy side of the campaign. PuckerUp4PH is about the disease and the patients and ensuring they're correctly diagnosed.
Question: What is PAH?
Professor Anne Keogh: We now understand high blood pressure and PAH is high blood pressure of the lung circuit. High blood pressure of the lung circuit is dangerous as it damages the walls of the arteries and people eventually become unable to breathe and go into heart failure, they then die of heart failure.
Question: Why are people who have PAH often not aware of it?
Professor Anne Keogh: Mostly because it has only been in the last decade that there have been therapies' and attempts to find patients with PAH.
About 3,500-4,000 people have PAH, in Australia and not even half of them are being treated; we know this from a Western Australia PhD study by Mr. Strange. He looked at what the magnitude in a certain population was and half the people in that population that had PAH were not being treated.
PAH is quite a hard disease to diagnose, unless the doctors are looking for it.
Question: How does PAH affect ones daily life?
Professor Anne Keogh: Breathlessness and tiredness- which is why PAH can be cheeky to diagnoses because everyone feels tired at times.
Question: What can PAH patients do to manage their lives?
Professor Anne Keogh: Mother's might have trouble looking after their kids and older people make have trouble with daily activities such as talking on the phone, showering and walking from room to room. Getting onto therapies and exercise programs can help with the symptoms of PAH.
Question: How can you manage PAH?
Professor Anne Keogh: Mainly with medication to bring the blood pressure of the lungs down. It is critical that a patient starts as soon as possible because if it is left unattended it has a bad outlook as most are dead within 2 or 3 years. It is important to hop in and treat PAH as soon as breathlessness arises.
Lupus and Scleredema sufferers and their specialists need to be aware of PAH and be checked out for PAH each year, by specialists looking and organising an echo soundwave test on the heart. 1 in 5 Scleredema patients have PAH. Lupus and Scleredema patients need to be aware of PAH and ask their specialist (cardiologist) to test for it. The echo soundwave test on the heart will point to or away from the diagnoses.
Interview by Brooke Hunter
MORE
- Chiropractic Myths & Truths
- Gerard Fogarty Arthritis and Knee Replacement...
- Kym Ellery The ELLERY Eyewear Collection Interview
- Dr Ross Walker The Real Modern Killers Interview
- Shelly Horton Hay Fever Help Interview
- Sebastian VanVeenendaal Royal Rehab's Beach...
- Abigail Koch Family Private Health Insurance...
- Monique Cashion Organic Awareness Month Interview
- Dr Bill Harris Omega-3s Interview
- The Top Ten Health Myths Busted
- Professor Bolin IBD Management a Life-Long...
- Anthia Koullouros Best Cold and Flu Defence...
- Leprosy in NSW
- Julie-Anne Mitchell Go Red for Women Healthy...
- Insight into Chronic Disease Hospitalisations...
- Jeff Chan Mobile Phone Allergies Interview
- How to Conquer Bad Winter Health Habits
- Bad Cholesterol Behind Cancer Spreading In Body
- New Screening Test Recommended To Help Prevent...
- Support For The Rural Nurse Workforce A...
- Kathy Nielsen Ovarian Cancer Australia National...